Haematology and BMT in Indore
Navigating the Complexities of Blood Disorders: Expert Haematology and BMT Care
Jupiter Hospital has emerged as a prominent private quaternary care facility and is home to our Haematology & Bone Marrow Transplant (BMT) department, offering specialised Haematology and BMT treatment in Indore. The centre's primary goal is to facilitate access to bone marrow transplants as a potential remedy for patients dealing with intricate blood disorders.
The core values of our dedicated transplant specialists at the Haematology and BMT hospital in Indore include innovation, collaboration, confidentiality, empathy, and integrity. With a robust track record, we have conducted numerous successful transplants for patients hailing from diverse regions across the world, all seeking solutions for a range of blood disorders.
We use a multidisciplinary approach to treat cancer and blood diseases, such as leukaemia, lymphoma, myeloma, and other conditions requiring transplants. Regardless of whether a patient is an adult or a child, our commitment is to create individualised treatment plans tailored to their distinctive and evolving requirements, ensuring comprehensive care before, during, and after the transplant.
Team
Looking for the Haematology and BMT in Indore
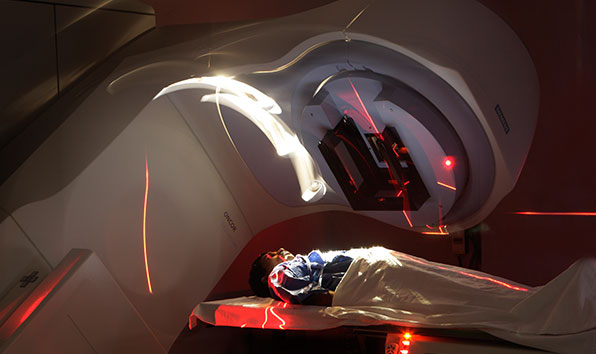
The Centre prides itself on its contemporary infrastructure and a team of experienced, internationally trained specialists. It is well-supported by transfusion services, laboratories, and a radiation oncology unit.
Prominent Features
Key features of the Centre include an exclusive unit unique to the city, round-the-clock Advanced Critical Care Services, spacious transplant suites equipped with HEPA filters, Adult and Care Units with isolation beds, outpatient daycare, and a comprehensive range of medical services, encompassing Chemotherapy, Immunotherapy, Blood Transfusion, Endoscopy, Bronchoscopy, and Dialysis.
Transfusion Medicine Services
The department operates 24/7, offering a variety of blood components, including platelet apheresis, NAT-tested blood components, peripheral stem cell harvesting, bone marrow processing, stem cell preservation through cryopreservation, and a Gamma Irradiator.
Extensive Laboratory Services
The Centre provides diverse laboratory services, such as Haematology, Flow Cytometry, HCA, Microbiology, Drug Assays, and Histopathology.
Treatment for Various Blood Disorders
The Centre specialises in the diagnosis and treatment of a wide range of blood disorders and blood cancers, covering conditions like anaemia, marrow failure syndromes, coagulation disorders, acute and chronic leukaemia, myelomas, lymphomas, myeloproliferative, and lymphoproliferative disorders.
Consultative Haematology Solutions
Our comprehensive services include Allogeneic and Autologous transplants using bone marrow, peripheral blood stem cells, and cord blood stem cells for both benign and malignant disorders.
A bone marrow transplant is a medical procedure conducted to replace a patient's unhealthy bone marrow with healthy bone marrow cells. This treatment encompasses bone marrow or peripheral blood stem cell harvesting and is often utilised in the management of various blood-related disorders, including leukaemia, lymphoma, and specific autoimmune conditions.
Significance of Bone Marrow
Bone marrow, a soft and spongy substance situated within the inner cavities of bones, plays a vital role in blood production. It contains tiny spaces that house primitive cells with the remarkable potential to develop into different types of blood cells. These exceptional cells are referred to as stem cells, possessing the ability to generate a variety of blood cell types, including red blood cells, white blood cells, and platelets.
Understanding the Two Types of Bone Marrow
In general, bone marrow exists in two forms: red and yellow. Most children predominantly possess red marrow, characterised by its richness in stem cells. However, as individuals reach adolescence, a significant portion of their bone marrow transitions to yellow marrow due to the infiltration of fat cells. Red marrow in adolescents is typically confined to specific bones, such as the hip bones, breastbone, ribs, shoulder blades, skull, spine, arms, and the ends of the thighs.
- Malignant Blood Disorders The application of bone marrow transplant or haematopoietic stem cell transplant plays a pivotal role in the diagnosis and treatment of malignant blood disorders. These conditions often require a combination of chemotherapy and specialised treatment modalities. These malignant disorders include:
- Acute Leukaemia (Myeloid & Lymphoid Leukaemia)
- Chronic Leukaemia (Myeloid & Lymphoid Leukaemia)
- Multiple Myeloma
- Myelodysplastic Syndromes
- Hodgkin’s and Non Hodgkin’s Lymphoma
- Myeloproliferative Disorders
- Neuroblastoma/Ewing’s Sarcoma, Medulloblastoma
- Treatment for Benign Blood Disorders: In addition to malignant conditions, bone marrow transplants are instrumental in addressing benign blood disorders. These non-cancerous disorders often require a tailored approach to treatment. They include:
- Thalassemia Major & Sickle Cell Disease
- Aplastic Anaemia
- Benign White Blood Cell Disorders - LAD/Congenital Neutropenia
- Immunodeficiency Disorders
- Severe Combined Immunodeficiency Disease
- Congenital and Pediatric Syndromes
- Other States of Bone Marrow Failure – PRCA, PNH, Fanconi's Anaemia
- Adrenoleukodystrophy
- Hemophagocytic Lymphohistiocytosis (HLH) - Both Primary and Secondary
- Hurler Syndrome
- Multiple Sclerosis/Scleroderma
The bone marrow transplant process exhibits variability, contingent upon the donor and the specific transplant procedures. In general, there are two central categories of transplant processes:
- Autologous Bone Marrow Transplant: In this method, the patient's own bone marrow or stem cells are harvested and cryopreserved for future utilisation.
- Allogeneic Bone Marrow Transplant: This method involves procuring bone marrow or stem cells from a donor. The donor may be a relative, often a sibling, or an unrelated individual whose bone marrow is HLA (Histocompatible Leukocyte antigen) compatible with the patient's. The transplantation of bone marrow typically takes place on the same day.
Diverse Allogeneic Transplant Types
A few of the different types of allogeneic transplants are the following:
- HLA (Immune)-Match Related Donor (Siblings) Transplant: The donor is typically a sibling whose HLA profile is a complete match with the patient.
- HLA (Immune)-Matched Unrelated Donor Transplant: The donor is unrelated to the patient but offers a complete HLA match.
- Haplo Identical Donor Transplant: The donor, often biological parents or half-matched siblings, supplies stem cells with a half-matched (haplotype) HLA profile.
- Umbilical Cord Blood Transplant: Stem cells extracted from a newborn's umbilical cord immediately after birth eliminate the need for an exact match. These stem cells are frozen and preserved for future transplant usage.
The Transplant Process
Following the harvesting, the bone marrow or stem cells undergo a filtration process to eliminate extraneous particles, primarily fat. Subsequently, they are taken to the laboratory for processing, including counting and screening, to prepare them for infusion.
Tailored Treatment
The choice of transplant type is meticulously guided by the patient's unique medical necessities, determined through professional medical evaluation. The overarching objective of the bone marrow transplant process is to address an array of blood disorders and particular cancer forms.
The Bone Marrow Transplant (BMT) journey is structured into three primary phases, each serving specific purposes and functions. These phases are:
Phase 1: The Pre-BMT Phase
The initial phase is centred around a comprehensive assessment and preparation of the patient. It includes a series of diagnostic tests, a holistic health evaluation, and the conditioning process to prime the body for the upcoming transplant.
Phase 2: Stem Cell Transfusion
In this stage, the actual transplantation takes place. Stem cells, sourced either from the patient's own body (autologous) or a donor (allogeneic), are transfused into the patient, marking a pivotal moment in the BMT process.
Phase 3: The Post-BMT Phase
The post-BMT phase is dedicated to monitoring and facilitating the patient's recovery. This includes vigilance against potential complications, continued immune suppression, and ensuring that the transplanted cells are properly engrafted success of the transplant.
Step 1: Preparation
The patient's journey embarks with their arrival at the BMT Centre. During this phase, the process unfolds with a comprehensive medical evaluation, the application of a multidisciplinary treatment approach, and the placement of a central venous catheter.
Step 2: Bone Marrow/Stem Cell Harvest
Stem cells are sourced either from the bone marrow or peripheral blood through apheresis. In the context of an allogeneic transplant, stem cells are derived from a donor, whereas an autologous transplant relies on the patient's own stem cells.
Step 3: Conditioning
The conditioning phase serves as the inaugural step in the transplantation process. It encompasses the administration of chemotherapy, radiation therapy, or a combination of both. The objective is to hinder bone marrow function to enhance the potential for disease cure. Some conditioning treatments may be conducted in an outpatient setting, potentially shortening the inpatient stay.
Step 4: Transplant
Right after the conclusion of the conditioning regimen, donor bone marrow or stem cells are infused, resembling a blood transfusion. This transition marks the inception of the post-BMT phase.
Step 5: Waiting for Engraftment (New Cell Growth)
During this phase, vigilant monitoring and supportive therapy are carried out for patients, with a particular focus on preventing infections.
Step 6: Engraftment and Early Recovery
Signs of new bone marrow or stem cell engraftment and development typically manifest around 2 to 3 weeks after transplantation. Monitoring and supportive care persist, while preparations for the patient's discharge begin.
Step 7: Long-Term Recovery
This phase entails the patient's release from the centre, discussions on ongoing clinical issues, and the process of reinstating their regular lifestyle. Patients are strongly encouraged to schedule regular follow-ups to preempt potential long-term complications.
Patients Speak
Hear the heartwarming stories of patients overcoming difficult afflictions
















 View Map
View Map Book an Appointment
Book an Appointment Find a Doctor
Find a Doctor Health Check-up
Health Check-up












 Find a Doctor
Find a Doctor Health Checkup
Health Checkup Book an Appointment
Book an Appointment